New approaches against metastatic breast cancer: mini-tumors from circulating cancer cells

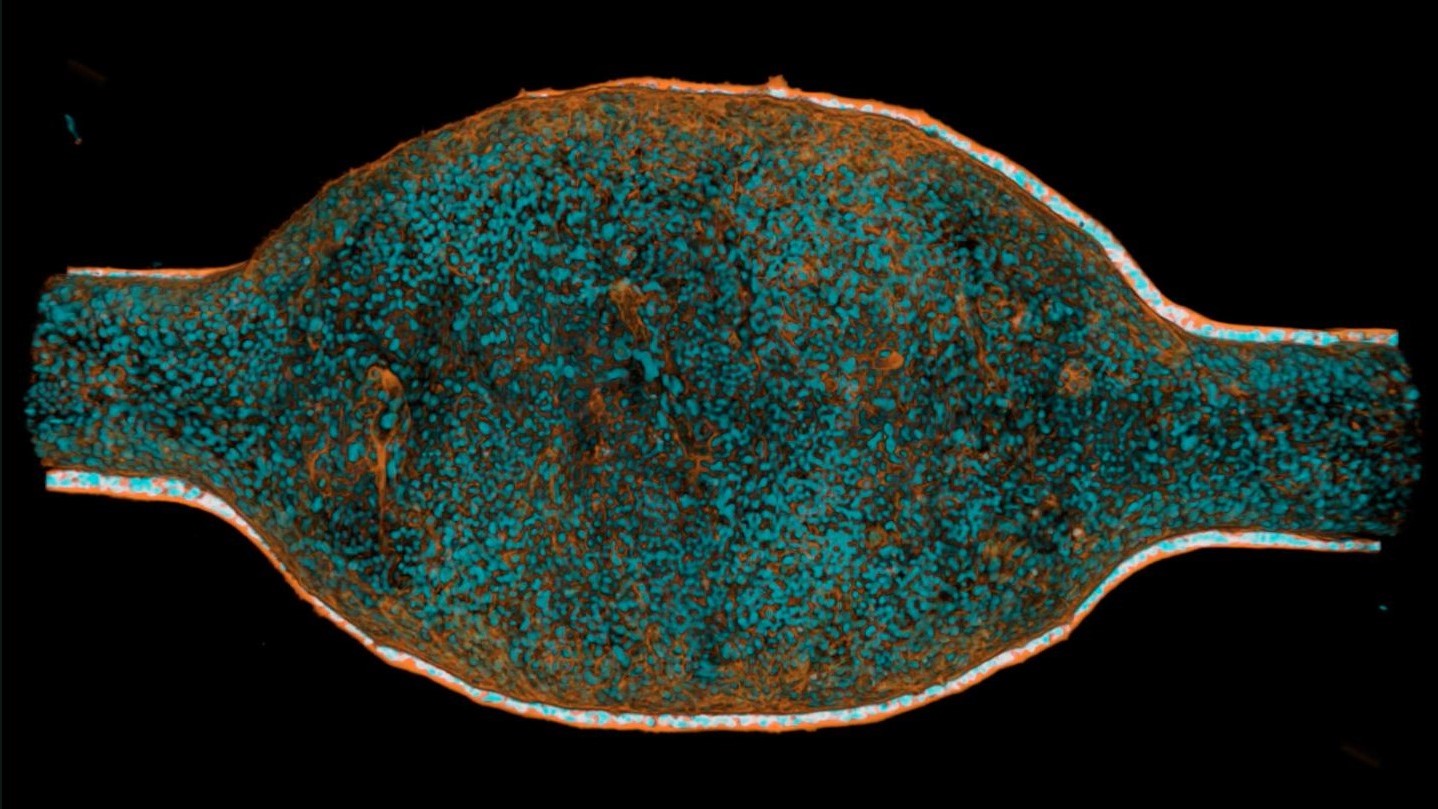
Tumor cells circulating in the blood are the “germ cells” of breast cancer metastases. They are very rare and could not be propagated in the culture dish until now, which made research into therapy resistance difficult. A team from the German Cancer Research Center (DKFZ), the Heidelberg Stem Cell Institute HI-STEM* and the NCT Heidelberg** has now succeeded for the first time in cultivating stable tumor organoids directly from blood samples of breast cancer patients. Using these mini-tumors, the researchers were able to decipher a molecular signaling pathway that ensures the cancer cells’ survival and resistance to therapy. With this knowledge, the team was able to develop an approach to specifically eliminate these tumor cells in lab experiments.
© Trumpp/DKFZ
Metastases are the dangerous offshoots of tumors that spread to vital organs such as the liver, lungs or brain and are usually difficult to treat. Even though the prognosis for breast cancer patients has improved significantly in recent decades, metastatic breast cancer still poses a major challenge, as the metastases often only respond temporarily to treatment.
Breast cancer metastases are initiated by cancer cells that detach from the primary tumor and migrate to other organs via the bloodstream. These circulating cancer cells (CTCs) are extremely rare and hide among the billions of blood cells. Andreas Trumpp, Head of a research division at the DKFZ and Director of HI-STEM, had already demonstrated several years ago that only a few of the circulating tumor cells are capable of forming a new metastasis in another organ. These mostly therapy-resistant “germ cells” of metastases are very rare, difficult to isolate and could not be multiplied in the laboratory until now. “This makes it difficult to develop targeted new therapies that directly attack the metastasis-initiating cells. However, if we understand how these cells survive the initial therapy and what drives their resistance, we could tackle the formation of breast cancer metastases at the root and perhaps one day even prevent them,” explains the first author of the paper, Roberto Würth from Trumpp’s lab.
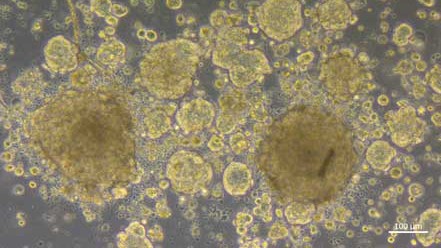
Andreas Trumpp’s team has succeeded for the first time in multiplying CTCs from blood samples of breast cancer patients and growing them as stable tumor organoids in the culture dish. Until now, this always required a detour, namely the complex and lengthy propagation of CTCs in immunodeficient mice. In order to understand how tumor cells become resistant to therapies, researchers need tumor material from different time points in the course of the disease. In contrast to surgical removal of tissue samples (biopsies), blood samples are simple and can be taken several times.
The three-dimensional and patient-specific mini-tumors can be cultivated from blood samples several times during the course of the disease and are ideally suited for investigating the molecular mechanisms that enable tumors to survive despite therapy. Preclinical tests on the efficacy of already available cancer drugs can also be carried out quickly and on a large scale on organoids in the culture dish.
In the clinical registry trial CATCH (ClinicalTrials.gov ID: NCT05652569) at the NCT Heidelberg, the genetic diversity of patients’ breast cancer cells is analyzed. Thanks to the successful cultivation of the organoids, Trumpp’s interdisciplinary research team, in close collaboration with the experts of the CATCH trial, was able to identify a key signaling pathway that ensures the growth and survival of breast cancer CTCs in the blood. The protein NRG1 (neuregulin 1) acts like a vital “fuel”. It binds to the HER3 receptor on the cancer cells and, together with the HER2 receptor, activates signaling pathways that ensure the growth and survival of the cells. What is also exciting is that even if this fuel runs out or the receptors are blocked by drugs, the cells find new tricks. An alternative signaling pathway, controlled by FGFR1 (fibroblast growth factor receptor 1), steps in and ensures growth and survival.
“With the help of such ‘bypasses’, tumors react to external influences, for example to targeted therapies against HER2. This is a crucial mechanism in the development of therapy resistance,” explains Roberto Würth. But there are ways out: the researchers used organoids to show that a combined blockade of both signaling pathways (NRG1-HER2/3 and FGFR) can effectively stop the proliferation of tumor cells and induce cell death.
Andreas Trumpp summarizes: “The possibility of cultivating CTCs from the blood of breast cancer patients as tumor organoids in the laboratory at different time points is a decisive breakthrough. This makes it much easier to investigate how tumor cells become resistant to therapies. On this basis, we can develop new treatments that may also specifically kill resistant tumor cells. Another conceivable approach is to adapt existing therapies in such a way that the development of resistance and metastases is reduced or even prevented from the outset. As the organoids are specific to each patient, this method is suitable for identifying or developing customized therapies that are optimally tailored to the respective diseases.” Before the method can be used to treat breast cancer patients, it must first be tested in clinical trials.
*The Heidelberg Institute for Stem Cell Technology and Experimental Medicine (HI-STEM) gGmbH was founded in 2008 as a public-private partnership between the DKFZ and the Dietmar Hopp Foundation
** The National Center for Tumor Diseases (NCT) Heidelberg is a long-term cooperation between the German Cancer Research Center, the University Hospital and the University of Heidelberg.
Roberto Würth, Elisa Donato, Laura L. Michel, Massimo Saini, Lisa Becker, Tasneem Cheytan, Daria Doncevic, Tobias Messmer, Ewgenija Gutjahr, Rebecca Weber, Corinna Klein, Hamed Alborzinia, Umut Yildiz, Vanessa Vogel, Mario Hlevnjak, Polina Kozyulina, Sarah-Jane Neuberth, Paul Schwerd-Kleine, Sevinç Jakab, Nicole Pfarr, Arlou Kristina Angeles, Astrid K. Laut, Darja Karpova, Mattia Falcone, Olaf Hardt, Benjamin Theek, Celina V. Wagner, Mirjam Becker, Sabine Wagner, Martina Haselmayr, Anita Schmitt, Carsten Müller-Tidow, Sabine Riethdorf, Klaus Pantel, Marc Zapatka, Holger Sültmann, Carl Herrmann, Verena Thewes, Peter Lichter, Andreas Schneeweiss, Martin R. Sprick, & Andreas Trumpp: Circulating tumor cell plasticity determines breast cancer therapy resistance via neuregulin 1–HER3 signaling
Nature Cancer 2025, https://doi.org/10.1038/s43018-024-00882-2